The Data Clarification Form Template for Clinical Trials That Works: Streamlining Data Integrity
Clinical trials are the lifeblood of medical advancement, but they are also incredibly complex undertakings. Ensuring the accuracy and reliability of data is paramount, and that’s where the humble yet crucial Data Clarification Form (DCF) comes in. This template is your key to unlocking pristine data, minimizing discrepancies, and ultimately, contributing to the success of your trial. This article provides a comprehensive guide to building a DCF template that truly works, optimizing your data quality and ensuring regulatory compliance.
Why You Need a Robust Data Clarification Form (DCF)
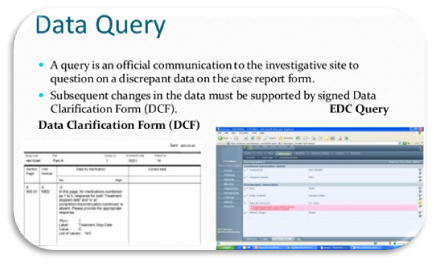
Data discrepancies are inevitable in clinical trials. Human error, ambiguous instructions, and complex protocols can all contribute to data that requires clarification. A well-designed DCF acts as a standardized communication tool, allowing you to:
- Identify and Resolve Discrepancies Efficiently: Proactively address data inconsistencies before they impact analysis.
- Maintain Data Integrity: Ensure the accuracy, completeness, and consistency of your trial data.
- Reduce Query Backlog: Streamline the query process, minimizing delays and maximizing productivity.
- Improve Data Quality: Enhance the reliability of your findings, leading to more robust conclusions.
- Support Audit Trails and Compliance: Maintain a clear record of all data queries and resolutions, vital for regulatory compliance.
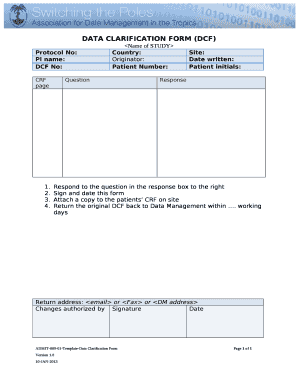
Key Components of a High-Performing Data Clarification Form Template
Creating a DCF template that effectively addresses data queries is crucial. Here’s a breakdown of essential elements:
1. Header Information:
- Trial Identifier: Clearly identifies the clinical trial (e.g., Protocol Number, Study Title).
- Form Number: Assign a unique identifier to each DCF for easy tracking.
- Date of Issue: Records when the DCF was created.
- Subject Identifier: Specifies the patient/subject related to the query (e.g., Subject ID, Visit Number).
- Investigator/Site: Identifies the site or individual responsible for responding.
- Source of Query: (e.g., Data Management, Statistical Analysis, Clinical Monitoring)
2. Data Query Details:
- Data Field/Variable Name: Clearly specifies the data point in question (e.g., Blood Pressure, Height, Adverse Event).
- Original Data Value: Displays the questionable data entry as it currently exists.
- Reason for Query: Describes the nature of the discrepancy. Be clear and concise. Examples include:
- Missing Data
- Out-of-Range Values
- Inconsistent Data
- Illegible Entry
- Reference Source: Citations the source document or data source where the original data was recorded (e.g., Case Report Form (CRF) page number, Laboratory report).
3. Response Section:
- Proposed Corrected Data Value: Space for the investigator/site to provide the corrected data.
- Justification/Explanation: Crucial for understanding the reason for the correction. This could include:
- A brief explanation of the correction.
- Reference to supporting documentation.
- The source of the corrected data.
- Date of Response: Records when the response was provided.
- Response Status: (e.g., Open, Closed, Resolved, Unresolved).
- Signature and Date: (If paper-based) for the investigator/designee to sign and date, confirming the accuracy of the response. In electronic systems, this may be an electronic signature.
4. Data Management/Quality Control Section:
- Data Management Review: Space for the Data Manager to review the response, verifying the accuracy and completeness of the response.
- Data Entry Changes: Record any changes made to the database based on the response.
- Data Management Signature/Date: Confirms the data management review and any changes made.
- Close-out Notes: Notes on the final resolution.
Best Practices for DCF Template Design
- Clarity and Conciseness: Use clear, unambiguous language. Avoid jargon.
- Standardization: Utilize a consistent format across all DCFs.
- Templates: Consider using pre-populated templates to streamline the process.
- Electronic Systems: Leverage electronic data capture (EDC) systems for integrated DCF functionality.
- Training: Provide training to investigators and site staff on how to complete DCFs correctly.
- Regular Review: Regularly review and update your DCF template based on feedback and evolving trial needs.
- Accessibility: Ensure the DCF is easily accessible to all relevant personnel.
- Version Control: Maintain version control to track changes to the DCF template.
Implementing Your Data Clarification Form Template
- Develop the Template: Use the components outlined above to create your DCF template.
- Integrate with EDC (if applicable): Integrate the DCF process seamlessly into your EDC system.
- Train Staff: Thoroughly train all personnel on the use of the DCF template.
- Monitor and Track: Track the number of queries, response times, and resolution rates.
- Analyze and Improve: Regularly analyze DCF data to identify areas for improvement.
Conclusion: Data Integrity Starts with a Strong Foundation
A well-designed Data Clarification Form template is an essential tool for ensuring data integrity in clinical trials. By implementing the components, best practices, and implementation strategies outlined above, you can streamline your query process, reduce errors, and ultimately, contribute to the success of your clinical trial. Investing time and effort in your DCF template is an investment in the quality of your data and the reliability of your results.
Frequently Asked Questions (FAQs)
Q: How often should I review and update my DCF template?
A: Review your DCF template at least annually, or more frequently if you identify recurring issues or if there are significant changes to your clinical trial protocol or regulatory requirements.
Q: What is the typical turnaround time for responding to a DCF?
A: Response times vary, but aim for a timely response, ideally within a few days to a week. This timeframe should be defined in your study protocol and DCF SOP.
Q: How do I manage DCFs in a multi-site clinical trial?
A: For multi-site trials, use a standardized DCF template, EDC system, and clear communication protocols. Establish a central point of contact for data queries and ensure all sites receive adequate training on the DCF process.
Q: What are the consequences of not addressing data discrepancies? A: Failing to address data discrepancies can lead to inaccurate study results, regulatory violations, and potentially, the rejection of your study data. It can also impact patient safety if inaccurate data informs clinical decisions.